Extended Health
Extended Health benefits are designed to help you pay for specified medical services and supplies, incurred by you and your eligible dependents, when not provided under a government health plan or by a tax supported agency.
Some of these covered expenses may include:
- Prescription drugs
- Vision care expenses – eye exams, glasses or contact lenses
- Paramedical practitioner visits such as chiropractors and physiotherapists
- Hospital room charges
- Emergency ambulance
- Medical Referral Benefits
- Out-of-province emergency medical and travel assistance
For a full list of what is covered, please refer to the Extended Health Benefits and Vision Care sections of the Health Benefits Plan Booklet.
NEW – Prescription Drug Prior Authorization Program Starting July 1, 2023
There are a number of prescription drugs which will now require prior authorization before they can be determined eligible under the Plan. The complete Prior Authorization Listing of these drugs can be found online at: https://www.telus.com/en/health/prior-authorization-forms
If your doctor prescribes a drug for you or one of your eligible dependents, that is on the Prior Authorization Listing, when you take your prescription to the pharmacy, your pharmacist will be advised that you must obtain prior authorization first. You will then need to download the applicable Prior Authorization (PA) form for that drug from: https://www.telus.com/en/health/prior-authorization-forms and complete the patient section, have the prescribing physician complete their section of the form, and then send the completed form to where indicated.
This information will be reviewed, and it will be determined whether the required eligibility criteria is met. The decision will be communicated directly with the patient or individual indicated by the patient on the form. If deemed to be eligible, an exception will be added to that patient’s Plan record so that the pay-direct card will accept that drug going forward according to the terms of the approval.
It's recommended that you refer to the Prior Authorization Listing while you are with your doctor, so that if a drug he/she intends to prescribe is on the Listing, the applicable Prior Authorization form can be downloaded, printed, and completed before you leave your doctor’s office. If you need assistance accessing a Prior Authorization form, you can contact the claims customer service department at D.A. Townley.
If the prescribed drug is one that must be coordinated with Provincial Fair PharmaCare under Special Authority, you will also be advised to ask that your doctor apply for Provincial Special Authority for that drug on your behalf. This will not impact your ability to fill your prescriptions if it’s approved under the Prior Authorization Program, but in order to ensure continued eligibility, the decision from Fair PharmaCare must be received by D.A. Townley within 90 days of the request.
How to File a Claim
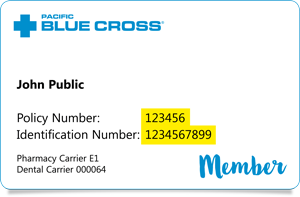
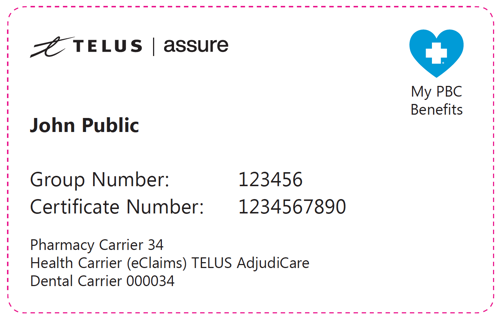
Some claims, such as prescription drug, paramedical practitioner visits or vision care expenses, may be able to be submitted directly to the Plan on your behalf so that you only have to pay your share of the cost. Present your Member ID card to your pharmacist, optometrist or your paramedical practitioners (such as a physiotherapist) at the time of your next visit.
If you paid the full cost of your expense, you can submit your receipt for reimbursement, either:
- through the D.A. Townley My Claims portal or mobile app. If you have not yet registered, do it today!
- using the Extended Health Benefits Claim form - The completed claim form together with copies of the receipts should be sent to the Administrator. You can do this by fax (604) 299-8136 or by email to health@datownley.com
- If you are coordinating the claim payment with your spouse’s health plan, you should include the primary carrier’s payment statement.
Any questions on completing the form can be directed to the Administrator.